David Eby - Saviour of Safer Supply?
With the heavy-handed BC Bill 36: The Health Professions and Occupations Act, is David Eby smoothing the way for “safer supply” super-concentrated Fentanyl and drug legalization?
Newly declared Premier David Eby wants housing quotas and yet another audit on the financial mismanagement by BC Housing. He wants to clean up the Downtown Eastside into a neighbourhood near you, by any means possible.
But where does David Eby stand on BC’s addiction problem and safer supply?
DECRIMINALIZATION
For decades, local drug advocacy groups have wanted drug decriminalization and legalization.
For years already, media and spokespeople have been indoctrinating us on destigmatization of drug use and safe supply - in fact, since 2017 when the BC Centre on Substance Use was created and Dr. Bonnie Henry published her decriminalization report “Stopping the Harm” - a report that ignored the fact that Portugal had immediately accessible drug treatment and psychological services in place before drug decriminalization.
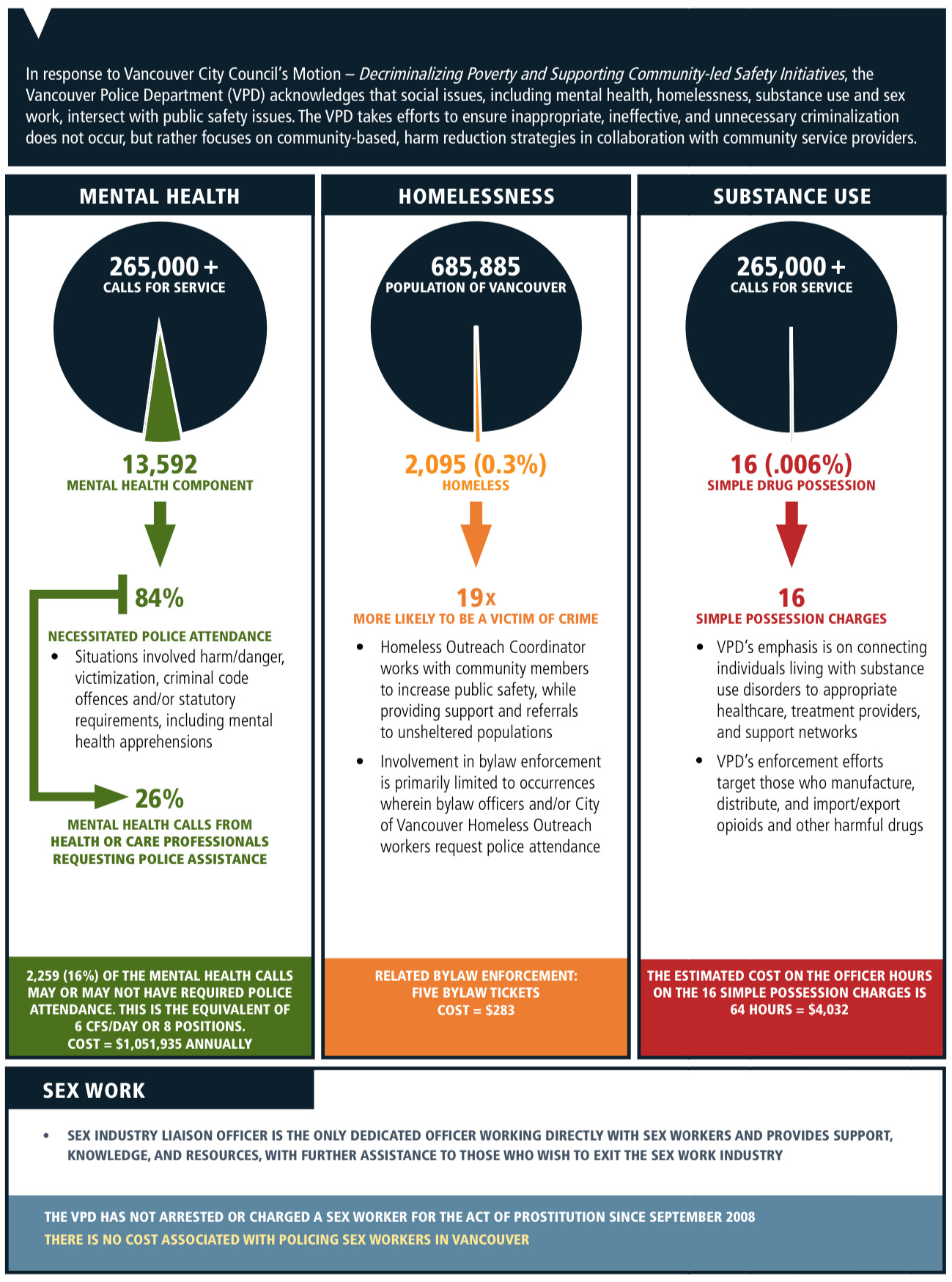
The Vancouver Police Department was rarely charging for drug possession, so the political posturing of decriminalization did not alter day-to-day reality.
Taken from page 69 of this VPD document.
As is the case in Oregon, decriminalization without treatment in place increases drug use.
BC has a proven track record of increasing the population with opioid use disorders, ever since Public Health took over addiction management in 2003.
Notice the increase by 40,000 people with opioid use disorders in BC between 2001 and 2017, and now there are between 60 and 100,000 people altogether if you talk to Drs. Henry, Gustafson and Sutherland. Their comments are further below.
CLOSING THE GAP on ‘SAFER SUPPLY’
The toxic overdose crisis has been ongoing since 2016. Before it was about Fentanyl pretending to be Heroin, and now it’s about Benzodiazepines contaminating the Fentanyl.
The Covid-19 Pandemic has championed the notion of safer supply Dilaudid 8 mg capsules (one “Dillie” is equal in strength to 9 Tylenol #3’s) to filter, cook and inject. There were complaints that they weren’t strong enough and didn’t satisfy. Dillies were sold to dealers in order to get the desired drugs. Dillies were then sold to novice users as “safe” drugs, or sold through the mail to the Yukon or Newfoundland. This testimony was provided by local physicians to the Alberta Safe Supply Hearing.
This U-shaped diagram on prohibition and regulation of substances by Dr. John Marks always gets cited by those in favor of drug legalization, like the PHO, the BCCDC and SFU’s Canadian Drug Policy Coalition. Dr. John Marks was a psychiatrist that prescribed Heroin in the UK in the 1980’s.
The declared, obvious solution is regulated, safer supply Fentanyl, which is in fact super concentrated Fentanyl in 250, 1000 and up to 10,000 mcg per capsule, potentially scalable to service up to 100,000 clients, as a means to combat the toxic overdose crisis.
Don’t worry. Soon it will come in child-proof packaging.
Clients won’t divert it because it will cost the same as street supply. Just don’t ask where clients get the money to pay for it.
People on chronic illicit opioids aren’t looking to get high anymore. They just want to prevent withdrawal. That’s why someone on daily 40,000 mcg of safer supply Fentanyl needs to use on top of that.
There will be less demand for criminally-sourced drugs.
Dr. Julian Somers estimated a 5 to 6 figure dollar range per year to supply one drug user with medical grade Fentanyl (Pages 44-45).
Safer supply Fentanyl even made the New York Times in a July 26th article and a Sep 2nd podcast.
And don’t forget the increased need for more supportive housing and inhalation overdose prevention facilities, as more people prefer to smoke than inject now.
Where will this take Vancouver, a long-time magnet for open drug use and homelessness ? With David Eby’s plan to grow Metro Vancouver by a million people, even more drug users will be welcomed to a warmer, friendlier climate for clean and possibly free drugs and free housing.
As said by Michael Schellenberger:
If you basically give people drugs to use and make their lives very comfortable to just use drugs all day, you’re effectively lowering the bottom whereas if you have consequences for behavioural disorders, including public drug use, public camping, public defecation, you may raise the bottom and help people to get into recovery.
Pierre Poilievre, just the latest person to speak out against safer supply.
Find out more in the Select Standing Committee on Health records on the overdose crisis, an outcome of the BC Coroner’s Death Panel Review Recommendations : (1) safer drug supply, (2) develop a 30/60/90-day illicit drug toxicity action plan with ongoing monitoring, and (3) establish an evidence-based continuum of care.
Closing the Gap, Reducing Barriers: Expanding the Response to the Toxic Drug and Overdose Crisis
So, it is no surprise that the summation report supports forcing more overdose prevention sites and supportive housing, without any defined supports or expectation of behaviour, into a neighbourhood near you. Quite the opposite of Portugal and the Netherlands, which are all about regulating behaviour, dissuading drug use and increasing personal responsibility.
Page 28:
With respect to supportive housing, the Committee emphasized the need for 24/7 wraparound supports for individuals dealing with substance use, which should include clinical support and take care of their daily needs. Members acknowledged that supportive housing initiatives often have trouble getting community support. Therefore, they discussed the creation of a toolkit of best practices to help operators build supportive housing and gain community support***. Further, Members discussed the need to have accountability measures in place to ensure that housing and supportive housing initiatives are being adequately resourced and are providing effective supports.
*** For more on gaining community support, refer to The Meaningless Words.
There is no definition for 24/7 wraparound supports. Even if they exist, some people don’t want them.
Most people don’t want disinhibited DTES behaviours exported into their neighbourhoods.
It’s time to retire the failed terminology of “supportive housing” and “tenant mix” since there is no government-accepted standardization of supports for people that need or want them.
Page 30:
Access to Harm Reduction Services
Several barriers to accessing harm reduction services were identified. Some organizations and individuals criticized certain municipalities for making zoning decisions and denying business licenses that limit where harm reduction facilities can be located, as well as for implementing bylaws that prevent carrying harm reduction supplies. The Fraser Health Authority noted that it has experienced significant municipal opposition to setting up fixed harm reduction services in some communities, including direct opposition to locating sites in downtown areas where they would most benefit the clients they are meant to serve.
Some organizations and individuals, including the Umbrella Society, the Drug Prevention Network of Canada, and Westminster House Society, suggested that the government is currently dedicating too many resources to harm reduction initiatives, at the expense of other interventions like prevention or treatment services.
Page 31:
Overdose Prevention Sites
According to the Ministry of Mental Health and Addictions, there are currently 42 publicly available supervised consumption and overdose prevention sites in the province, and since 2017, there have been more than 3 million visits to these sites.
Pivot Legal Society pointed to order M-488, issued by the Minister of Health in 2016, which required that overdose prevention services exist throughout the province and noted that this order is not currently being met.
The Committee heard about additional limitations, including the services provided at these sites. Several submissions noted the increasing number of individuals who prefer to smoke or inhale substances rather than to inject or ingest them; however, supervised consumption and overdose prevention sites rarely include facilities for smoking or inhaling substances. The Ministry of Mental Health and Addictions indicated the expansion of inhalation facilities is a current strategic priority, and that 13 sites have been established. The People with Lived and Living Experience Committee shared that supervised consumption sites are designed to help opioid users, and therefore the environment is not conducive to stimulant use.
The Ministry of Mental Health and Addictions shared that, by providing information about drug contents, drug checking allows individuals to make informed choices about their use of substances, provides an opportunity for referral to other harm reduction services or the health care system, and supports surveillance of the illicit drug supply and identification of trends.
The City of Vancouver has no restrictions on where any of this can occur because that would be discriminatory and against the Human Rights of the drug user.
The opioid crisis panel obviously didn’t take a tour around the Yaletown OPS with its open drug scene, or be educated on how other countries got their open drug scenes under control.
Aside from indigenous groups looking at the overall impact of addiction and overdoses on their communities, the BC government panel didn’t acknowledge the much larger, growing problem of addictions and addiction behaviour in BC, the negative impact they have on our society, and how the panel recommendations could potentially worsen both addiction behaviour and society.
From the overwhelmingly safer supply-positive BC overdose crisis hearing, you will understand why Marshall Smith, heavily featured in “Vancouver is Dying,” up and left BC for Alberta. Even Dr. Perry Kendall had to comment that the BC Centre on Substance Use did not want to listen to Smith’s abstinence-based approach.
As suspected, in BC there is systemic bias against abstinence-based treatment, such as with Sancta Maria House and Recovery-Oriented Housing.
The excerpts that follow are faithful to the audio recordings in the embedded links.
DR. BONNIE HENRY WANTS DRUG LEGALIZATION
Dr. Henry was careful to not identify what safer supply is, but did declare her support for drug legalization and dismissal of abstinence-based treatment.
She used all of the expected buzz words featured in her Stopping the Harm report about prohibition, destigmatization, decriminalization, criminalization of poverty, racism, etc.
Except for one of her lines quoted in the YouTube documentary “Vancouver is Dying,” the media didn't report on any of Dr. Henry’s presentation on the overdose crisis and accompanying answers:
The other part of it is: how do we meaningfully get access to non-prescribed drugs of a known potency that people can use? We can't stop people from using drugs right now. We estimate people with substance use disorder — so that's problematic use of substances and drugs — is about…. There are probably 60,000 people in British Columbia, and they're not all accessing treatment. Not everybody is at that place where recovery is an option. We're also learning that everybody's recovery journey is unique because of where they've come from in their background and their life.
Not to disparage our colleagues, but there's still a basic understanding that abstinence is the only way to treat things, and that's based on alcohol. Abstinence is an important treatment modality for people who have addictions to alcohol, but it does not work for opioid addiction, because it is a chronic, relapsing brain disease. We know that abstinence, especially in the same ways that we did it with alcohol, just doesn't work for people who have a dependency on opioids.
It has been a challenge to get the colleges on board. There's a lot of concern about use and prescribing of opioids, so they have been focusing mostly on opioid agonist therapy — Suboxone. But I am working with them to push them to have what I call a protocolized model. So somebody can come in to an overdose prevention site, they can talk to the peer or the people who are working there and be able to access a supply of drugs that would keep them from using the street supply in a way that is safe for them. These are things that we need to work on, for sure.
So, Dr. Bonnie Henry is pressuring the College of Physicians and Surgeons of BC and the BC College of Pharmacists to allow for easy access to recreational drugs after they’ve made effort to curb the medical prescribing of opioid medication after the Purdue OxyContin Opioid Addiction Crisis. And after the BC Government sued Purdue Canada for opioid damages, for a prescription drug less potent than Fentanyl.
According to Dr. Kendall, it was the College of Pharmacists that was tough on safe supply.
How convenient is that on Nov 24th, the provincial government has passed Bill 36: The Health Professions and Occupations Act so that the government can appoint every member of the Board on the College of Physicians and Surgeons of BC and BC College of Pharmacists without allowing their members to elect Board members anymore.
I believe — and my colleagues and the medical officers of health in this province have written a report on this — that yes, we should go to legalization of these substances. It is the illegal drug market that is fuelling the toxicity and the criminal elements that feed off that as well. But we're not…. As a society, I don't believe we're at that place yet.
Dr. Bonnie Henry thinks smoking Fentanyl is good:
What we've seen is — in one way, it's a good thing — that people prefer smoking substances now. Particularly with people who are using fentanyl, it's gone up from about 60 percent to 80 percent of people who are now smoking rather than injecting. In some ways, that's good. In other ways, it makes it challenging, because our overdose prevention sites are not set up, in most of the places, to deal with people who are smoking drugs. The worry is the impact on people around them, especially staff and peers who are working in those overdose prevention sites.
If people like smoking so much, why are there so many discarded needles?
From Dr. Henry’s presentation.
We don’t want staff overdosing in inhalation tents. Imagine the WCB claims.
Michael Schellenberger, in his comments to the Alberta Safe Supply Panel, does not think smoking drugs is good:
Now, on this issue of stigmatization, even more than just stigma I think we should be frightened of these drugs. Methamphetamine and fentanyl are extremely – these are some of the most toxic, intoxicating, addictive, and deadly drugs ever invented. They make the heroin and cocaine epidemics of the past look like child’s play in comparison. I mean, the poly drug use is rampant. When I interview homeless people – and I’ve been continuing to interview them in recent weeks, as I have for months before the book came out – people are using methamphetamine and fentanyl combined, and they’re smoking them all day long. That’s incredibly destructive, and we should be afraid of that.
Far more concerning are the “evidence-generating” words of Dr. Réka Gustafson from the BCCDC.
Opioid agonist therapy is the current evidence-based treatment for opioid use disorder.
What you will see is that although opioid agonist therapy is the evidence-based treatment for opioid use disorder, the retention in that treatment is extremely poor in our population.
What you'll see in the little graph on the right side is a study that demonstrates that, for those who are on opioid agonist therapy, it remains protective against death, even in the context of the fentanyl contamination of the drug supply. But a very, very small proportion of people are retained on this treatment.
Dr. Gustafson’s graph on the left suggests that OAT is failing.
However, from the cited paper on the right on the overdose protective effect of OAT:
Opioid agonist treatment (OAT), primarily with methadone or buprenorphine/naloxone, is a safe and effective treatment for opioid use disorder that has been shown to suppress illicit opioid use and reduce the risk of death. A recent systematic review and meta-analysis of observational studies conducted between 1974 and 2016 found that being on treatment was associated with a lower risk of death from all causes and from overdose.
Dr. Gustafson didn’t take into account the effect of "safer supply” on OAT retention.
As quoted from a BC addictions physician that participated in the Alberta safe supply hearing:
With safe supply that kind of went out the window. Many of our patients scattered. Many did not come back. A few did. They are basically either lost to follow-up, you know, and we’re not getting the new patients to replace them because now on the street you can get anything, any time, anywhere.
There is no recognition for the lack of pressured support towards societal re-integration like that used in Portugal and the Netherlands, and the influx of drug users into the province since the onset of the pandemic.
Public health officials and those in favor of safer supply like to quote this part:
The risk of death was highest in the first four weeks after stopping treatment (32.0 deaths per 100 000 person years on methadone and buprenorphine/naloxone), with a swift decline in the risk of death observed thereafter. These findings are important because people frequently stop and start these medications, and this exposes them to repeated periods of high risk of death. Excess mortality after stopping treatment can be explained by a loss of tolerance to illicit opioids during treatment, which increases the risk of fatal overdose after resuming illicit opioid use.
“Explained” but not proven. Suboxone (buprenorphine/naloxone) blocks other opioids from attaching to opioid receptors. A lot of opioid would need to be used on top of Suboxone in order to get a high. Wouldn’t the loss of protection from Suboxone contribute towards opioid overdose?
Dr. Gustafson went onto discussing dispensing Fentanyl in a non-medicalized way, pressuring Colleges, and evidence generation.
These services (OAT) are also a very high barrier to a number of individuals. It misses those who do not access health care or who do not want a record of their substance use. Daily pickup at a pharmacy is highly disruptive compared to the access to the illegal market. It essentially traps people in a system that does not allow them to manage their lives and manage their substance use in the context of a life that contains all sorts of other things that are important for individuals — work, social connections and, really, just participating in society.
(Notice that this narrative intentionally excludes monthly injected Sublocade, a long-acting version of Suboxone, which eliminates the need for pharmacist observed use. Check out the remarkable success story in Timmons, ON.)
The other challenge we have at this time is that the regulatory bodies and federal and provincial policy frameworks really have not kept up with the need for innovation to address the rapidly evolving drug toxicity crisis.
(Sublocade is an innovation, as well as, unexplored in Canada, injectable Naltrexone and future Fentanyl vaccines mentioned below.)
One of those interventions that I will just describe in a bit more detail is this enhanced access model, which the Portland Hotel Society has implemented recently. It does take us, again, incrementally closer to the public health vision of a tightly regulated market. Purchasing the substances is a key component.
It consists of a physician assessment of the risk of overdose. Again, it's the physician assessment of the risk of overdose. Are you at risk of dying?
(And you can’t overdose on or divert regulated, take-home Fentanyl?)
Then a prescribed, pharmaceutically manufactured and compounded powdered fentanyl for witnessed consumption, eventually moving to a prescribed and pharmaceutically manufactured compounded powdered fentanyl for at-cost purchase for take-home.
These enhanced access and other paid purchase models have important advantages that I'd like to spend a little bit of time on. They vastly reduce the incentives to diversion, particularly the more harmful types of diversion. There's real-time feedback on consumer preferences that drive evidence and innovation.
(They aren’t patients anymore, but consumers with preferences.)
It incentivizes treatment of addiction, because the treatment substances are available for free for individuals.
(Better access to Fentanyl will increase uptake of Methadone, Suboxone or Sublocade? Or is Fentanyl the treatment now?)
If you've got purchasing medication, and there's an alternative that you're not purchasing, that's an incentive. It does not encourage increasing dependence on high doses of the drug.
(The very short half-life of Fentanyl promotes more frequent use and increases the risk of addiction. Even Heroin is better with an 8 hour half-life.)
It does not preclude making prescribed products available at no cost to select populations. It requires less medical oversight for each individual enrolled and has greater capacity. As you know, capacity is one of our rate-limiting steps.
It's available to those who do not meet the criteria for a diagnosis of a substance use disorder.
(More consumers!)
It functions within a current regulatory and legal environment. It is critical, therefore, to maintain the option to purchase at cost for take-away doses. That's a policy decision that is actually being currently considered, of adding some of these medications to the provincial formulary.
Counterintuitively, that may actually close the path to a scalable model that's available to a larger number of individuals. So I really do encourage you, before making any such a policy decision, to engage, in a meaningful way, the people who are actually delivering these services to ensure that a well-intentioned policy doesn't actually close the path to a sustainable and scalable model of providing individuals with care.
The potential for these public health models…. Really, they're the only models that can scale to the magnitude of the issue. There is no capacity in our current health care system to provide a medical model that will scale to the magnitude of the issue. It's also not just a medical issue. Therefore, medicalizing this issue does not necessarily solve the problem. These kinds of public health models would need to be subject to real-time, independent evaluation and feedback, and feedback from participants, to generate evidence in a rapidly evolving drug toxicity crisis.
(Public Health doesn’t practice medicine? The truth is revealed!)
You will often hear the term that some of these things aren't evidence-based. Not all of them are. Many of them are evidence-generating. The real advantage of both implementing and evaluating these programs in real time is that we can adjust to a rapidly evolving toxic drug market.
Former PHO Dr. Perry Kendall's dream of Heroin safe supply is antiquated compared to Dr. Christy Sutherland's dispensing of Fentanyl at PHS.
From Dr Sutherland's presentation:
When we look at the research, most of the research for opioid use disorder was done in a heroin context, and our context has changed to fentanyl. So it makes sense to me that these drugs that are old didn't work anymore. I wanted to change to PEP fentanyl, which is what we've worked on over the past few years, but it's a very challenging molecule. I can really understand how organized crime has killed so many people, because the molecule itself is incredibly hard to work with in the community setting as well as in hospital. The formulations we have are not strong enough for what my patients need, and the volume that we'd have to give them is just too high.
The fentanyl powder I wanted to talk about specifically, because it's a new protocol. Our team of nurses, pharmacists and physicians partnered with a national pharmaceutical supply chain company and compounding pharmacy to create a new way to deliver fentanyl in community at much higher doses than ever done before.
If I went to the hospital with a broken leg, they would give me 12.5 micrograms of fentanyl. I have patients on 40,000 micrograms in one day, injecting. The dosing is astronomical. I was talking with an anesthesia colleague. It's more than she uses in a month in the OR at St. Paul's — in one day, one person. So working on the supply chain and the lab to validate these doses has just been so challenging. No wonder my patients are suffering, right? They are even still using on top of what I'm giving them, and still in withdrawal.
We're trying to create safety with this system. For me, I want safety for the public, and I want safety for my patients. That's why we created this enhanced access program. It's a sales program that runs in parallel with the medical model.
The medical model is based on iOAT and TiOAT, all of our other interventions that we had been offering, where it's all observed dosing. But I don't go to my doctor to get observed alcohol, and a lot of my patients don't want to come see us, even though we're very nice. I don't take it personally that they don't want to see me to observe their doses. Fentanyl has a very short half-life, although it can accumulate in the fat and then become sort of a long-acting drug. But people use at night; they don't just use eight to four, the hours that we're open.
The work flow is very similar to everything else we've established before. It's a physician assessment, a documentation, a urine test, a PharmaNet check, a consent process. Everyone goes through a specific titration with a nurse to get to their specific dose. It's a decision-support tool that the nurse uses based on our protocol, where people have escalating doses until they say: "Here. I'm at the right dose." We haven't got there yet. We don't know what that right dose is going to be, because it's higher than what our supply chain can supply at this time.
PHS acts as the agent for the patient, so we purchase the drugs on their behalf and then try to recoup our costs. We are not making money, but it's easier for our pharmacy. Physicians are paid an hourly rate — I'm not making any money — and the nurses as well.
We wanted to make it as easy as possible for the patients. They can do partial purchasing. They can have prepaid tabs on file. Family members can pay. They can pay cash or credit card.
One of the other safety systems we put in place is that if someone wants to increase their dose, they have to come back and have it witnessed. Because I'm always conscious of my vulnerable patients being taken advantage of by organized crime — to say: "Dr. DeBeck, you go sign up for that program, then I want 30,000 a day from you" — I have to observe that person take it, to know that they're able to tolerate that dose.
The regulatory system for opioids doesn't exist right now. Right now it's individual prescribers deciding what is the right clinical plan for their individual patients based on evidence that's out of date and a lack of guidance, really. So our team created the regulations that we think should be in place. We priced it at the same amount as the illicit market so that it does not have resale value.
For the patients, it's how much money they were spending anyway, so it's no change for them. That decreases the risk of diversion, decreases the risk of organized crime hijacking the program. Then there is significant benefit to the patient, where they have autonomy, they're treated with dignity, and they know what they're taking.
Then we have an independent evaluation, by the BCCSU (the consumer group with lived experience) that the dose increases after the initial titration are observed. The policy and procedures are hundreds of pages long. We had a legal review by Arvay Finlay, so we meet all of the legal regulatory requirements, federally and provincially, for all three colleges. All three colleges had very positive receptions to this program. I met with nursing, physicians and pharmacy.
One of the keys to this is that fentanyl powder is not covered under PharmaCare. If it becomes covered under PharmaCare, I can't sell the drug. Then we are locking ourselves into a medical model, saying that we're having to urine drug test 100,000 people, because that's how many people would need this intervention. To have clinical eyes on those 100,000 people doesn't exist. There's no capacity in B.C. to do that.
(In BC, 100,000 people need safer Fentanyl? Compare that to the Netherland’s 120 people on Heroin maintenance. And the safer supply has to be Fentanyl because BC has created people that can tolerate 40,000 mcg of Fentanyl?)
ALTERNATIVES to “SAFER SUPPLY”
Alberta, who has turned its back on “safer supply” and looked towards recovery-oriented treatment and treatment communities, is reporting fewer overdose deaths. Either their plan is working, or more Albertans are coming to BC to overdose here.
Safer Fentanyl for drug users. Safer who knows what else. Safer and more inhalation centres for Fentanyl and Methamphetamine coming to a neighbourhood near you.
Safer Fentanyl, costing up to 5 to 6 dollar figures per user per year instead of monthly injectable Sublocade that is protective against overdoses and manages addiction.
From the CADTH Canadian Drug Expert Committee:
BUP-ER (Sublocade) is available as 100 mg and 300 mg single-use pre-filled syringe at a submitted price of $550 for either dose. At the manufacturer’s submitted price, the annual cost of treatment with BUP-ER is $6,600.
Or, not approved for use in Canada yet, injectable Naltrexone that blocks opioid receptors altogether.
Don’t you want to know who owns this mystery pharmaceutical company producing super concentrated Fentanyl powder?
Even better from a Public Health perspective is the emerging Fentanyl vaccination. As the activists have proclaimed that the overdose crisis has taken more lives than Covid-19, the production and distribution of the Fentanyl vaccine should be accelerated to meet the need for this crisis.
Imagine personal and societal benefits of redirecting the expense of safer supply and inhalation consumption sites to addiction treatment, rehabilitation and recovery-oriented housing.
Even more mega millions would be available by downsizing bloated bureaucracy and going back to evidence-based treatment instead of the optimistic, evidence-generating kind.
Members of Chinatown and the VPD are trying to fight back against the insanity of the DTES, but they don't have a concept of the future expansion of the drug market, its new participants and increased locations to facilitate drug consumption in Vancouver.
Will David Eby move past his counterculture ways and listen to reason? Or more likely, will he double down and find more ways to control and micromanage our lives with housing, health care and safer supply coming soon to a neighbourhood near you.
The next election can't come soon enough.